SLAP Lesions
SLAP (Superior Labral Anterior-Posterior) Lesions refer to tears of the labrum (the ‘meniscus of the shoulder’) near the top of the glenoid socket. SLAP lesions detach the base of the Long Biceps Tendon, as the Long Biceps Tendon essentially originates from the top of the labrum. SLAP lesions usually occur in young overhead athletes, especially throwers and swimmers, but can occur in people of any age from trauma, such as a fall, motor vehicle accident, skiing, etc. In throwers, a tight shoulder can predispose to a SLAP lesion, and it is very important that pitchers keep their throwing shoulder stretched. Most athletic trainers are now fairly savvy about this and use the “sleeper stretch” on their pitchers to prevent SLAP lesions.
Typical symptoms of a SLAP lesion include soreness, pain and tightness in the back or outside of the shoulder. There may occasionally be a snapping or catching sensation. Throwers may experience the “dead-arm” syndrome, i.e. a loss of control and velocity.
It should be understood that a history, physical examination and MRI are not reliable for the diagnosis of SLAP lesions. Many times MRIs are ‘over-read’, meaning that a SLAP lesion is reported to be present, but is not really there, i.e. a ‘false positive’ reading. In many cases, the SLAP lesion is a ‘red herring’, and not the cause of the shoulder pain. Because of this, even if a SLAP lesion is suspected, the initial treatment should be non-operative, including rest and strengthening of the shoulder muscles. Throwing athletes should have their shoulders stretched, as above. If the shoulder symptoms persist after 3 months of strengthening, surgery can be considered. The exception to the three month rule is if there’s a painful snapping with shoulder motion or shoulder use, signifying that a mechanical issue is present inside the shoulder; these patients may consider surgery earlier.
In young athletes, an Arthroscopic SLAP lesion Repair has >95% success rate. Early motion is started after surgery to decrease the chance of stiffness. However, SLAP lesions usually do not cause pain in patients over 40-50 years old. Pain in patients over this age is much more commonly due to Rotator Cuff problems. In addition, repairing SLAP lesions in patients over the age of 45-50 years often leads to painful stiffness. So, if a SLAP lesion is causing problems in someone older than 45-50 years, it is often preferable to leave the SLAP lesion of the labrum unrepaired in order to avoid complications, and to simply perform an Arthroscopic Biceps Tenodesis. An Arthroscopic Biceps Tenodesis takes the Long Biceps Tendon off of the SLAP lesion / top of the labrum and stabilizes the Biceps Tendon near the humeral head. This gets the Long Biceps Tendon out of the shoulder joint so that it no longer causes pain, while allowing it to still move the elbow normally. Please see the “Biceps Tendon Disorders of the Shoulder” section for more information.
Arthroscopic Biceps Tenodesis
After surgery, keep the arthroscopy portals (stab wounds) clean and dry for 24 hours. Before 24 hours, bathing is fine; just keep the shoulder above water and don’t get the dressings wet. After 24 hours, the wounds can get wet in the shower, just blot them dry. Don’t submerge the wounds under water until the stitches are removed, which usually occurs at roughly 2 weeks. The elbow, wrist, forearm and hand can all be moved early on, to prevent stiffness. During Shoulder Arthroscopy, fluid is placed into the shoulder. This fluid will leak out over the first 2-3 days, and is not blood. SLAP repairs have a tendency towards stiffness, so motion and therapy are often begun early, after one week.
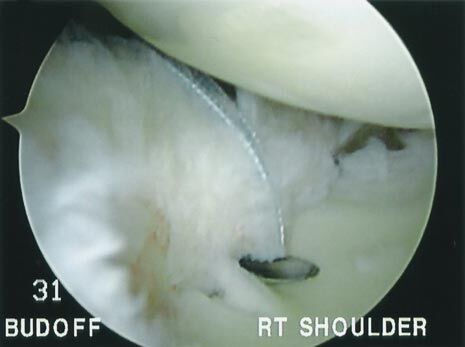
A SLAP lesion: The Top of the Labrum Has Been Torn Off of the Glenoid Socket
Suture Anchors (Little Plastic Harpoon-Heads With Sutures Attached to Them) Are Placed Into the Bony Glenoid Socket
A Suture Passing Device is Placed Around the Labrum / SLAP Tear
The Anchor’s Suture is Tied Around the SLAP Tear, Fixing it Back to the (Glenoid) Bone it Tore Off From